Fibroids also known as uterine leiomyomas have become a hot topic on social and traditional media over the last couple of years. In the medical community, we are ecstatic that more people are learning about a condition that will affect 80% of Black and 70% of white women by the age of 50 (Baird, 2003). Consequently, you may have come across posts that made you wonder if you in fact have fibroids. You have started paying attention to the patterns and nuances of your cycle. At this point, you’re not sure. Are your periods normal or should you in fact be concerned about your abnormal periods?
What are Fibroids
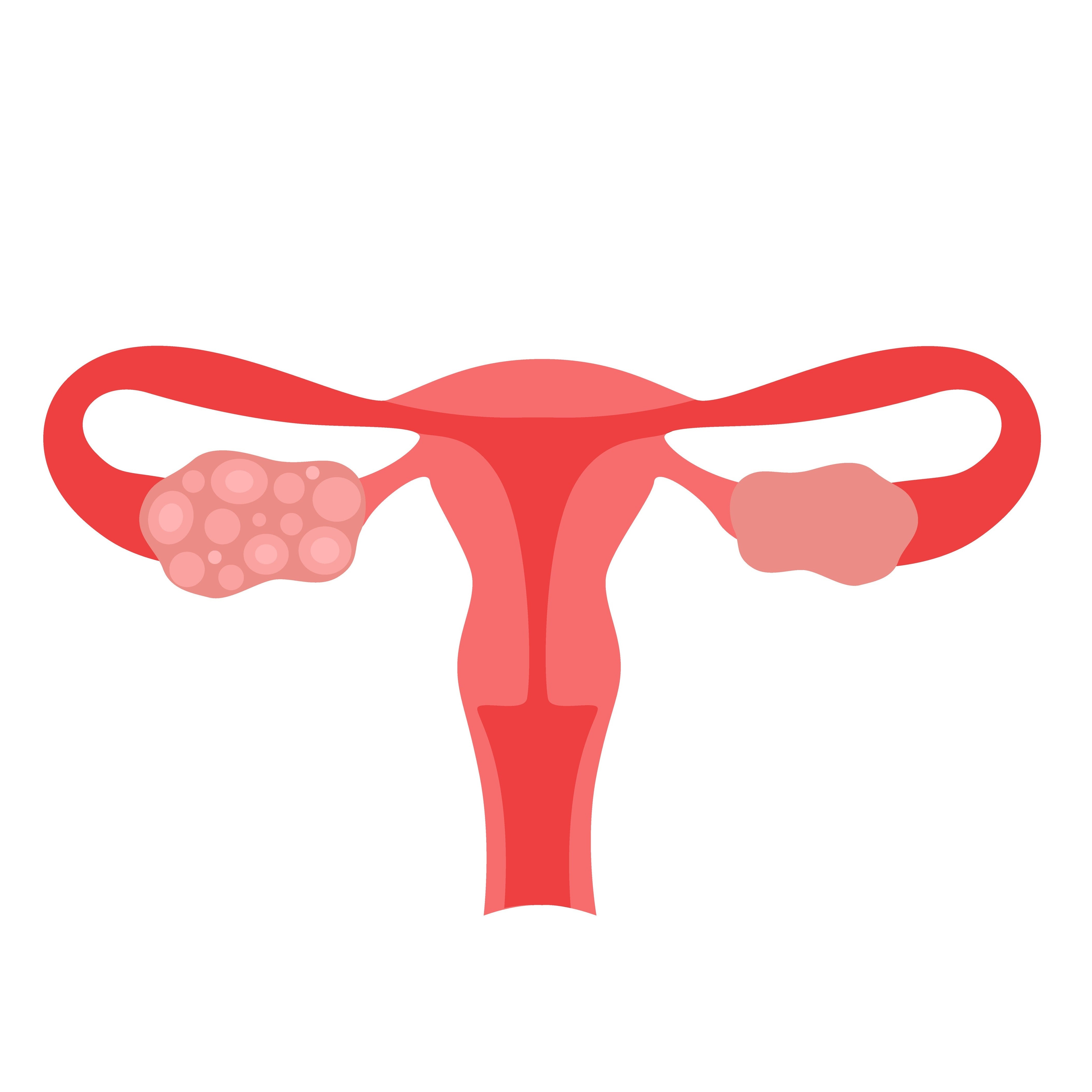
Fibroids are a non-cancerous tumor of the smooth muscle portion of the uterus. They are the most common benign tumor of the female reproductive system (Eltoukhi, 2014). Of the women that have fibroids, only 20-50% will experience symptoms (Eloukhi, 2014). As mentioned earlier, Black women are at increased risk of having fibroids. In addition, Black humans with vaginas are diagnosed with fibroids at younger ages, have more invasive symptoms and have larger sizes and numbers of fibroids (Jacoby, 2010). Consequently, those humans are being offered terminal surgery that ends reproduction such as a hysterectomy (removal of the womb surgically) at a rate higher than individuals of other races (Wechter, 2011). Fibroids primarily cause abnormal vaginal bleeding that is characterized by heavy and/or prolonged periods. Normal menstrual cycles occur on average every 21 to 35 days, last 3- 7 days and result in 80 ml of blood loss per cycle.
Symptoms of Fibroids
Heavy Bleeding
It is difficult to quantify 80 ml of blood loss when using feminine hygiene products. Many of us equate accidental blood strike through on clothes as a sign of heavy bleeding. The bleeding cycle of a woman can change slightly on a month to month basis. The most common reason for menstrual blood accidentally staining clothes is in truth inappropriately chosen absorption level and/or application of the feminine hygiene product. When using a product with the appropriate absorption levels, having to change an item in less than two hours when fully saturated or full (in terms of a menstrual cup) is concerning and would require a medical evaluation. The pattern of one cycle usually does not provide enough information for a healthcare provider to make a determination of the nature of your cycle. The minimum amount of time required to make a full evaluation unless your bleeding pattern is extremely heavy is 3 cycles or 3 months. It is advisable to track your periods for 3 months prior to a medical appointment to discuss your concerns about your menstrual cycle.
Bulk symptoms
Uterine fibroids also cause a set of symptoms known as bulk symptoms. Bulk symptoms are due to the volume of the tumor. They can cause pelvic pain and pressure with or without a cycle, dysmenorrhea (painful periods), urinary frequency as an anterior fibroid presses on the bladder, changes in bowel movement that may include constipation plus/minus bouts of diarrhea as a posterior fibroid compresses the intestines, pain with intercourse, increased abdominal circumference and weight gain in the lower extremities as the weight of the uterus impairs lymphatic drainage. These uterine fibroids symptoms should be recognized and shared with your Gynecologist.
Fertility
Fibroids have also been associated with subfertlity especially if the fibroid is submucousal or near the lining of the uterine cavity. The fibroids can interfere with the path of sperm, fertilized egg or implantation of a fertilized egg. In addition, it may interfere with the blood supply of a developing zygote. Fibroids can also increase the risk of a miscarriage or preterm birth. Women that have fibroids at the time of pregnancy are at risk for bleeding and pain during the pregnancy. Women who have had uterine sparing procedures for the treatment of fibroids prior to pregnancy may be directed by their surgeon to have a Cesarean delivery as the uterine scar(s) from the procedure may not withstand the forces of uterine contraction during labor.
Testing for Fibroids
When you decide to get checked out for fibroids, what should the process consist of? Basic laboratory tests should obtain a sample of your blood which is analyzed for a complete blood count to determine if you are anemic, thyroid stimulating hormone to rule out concomitant thyroid disorders that can cause abnormal bleeding and vitamin D levels as women with fibroids have been determined to have vitamin D deficiency with <20-30 micrograms/ IU. In addition you should have radiologic imaging to visualize your cervix, uterus, uterine cavity and ovaries, The most common imaging study is a combination abdominal and vaginal ultrasound. Other options are Magnetic Resonance Imaging (MRI), saline sonogram, hysterosalpingogram (HSG), and/or hysteroscopy. Of note, abdominal x-rays and Computed tomography (CT) are not particularly useful in studying fibroids. A complete assessment of fibroids should conclude with a discussion of the presence, number, location and size of each fibroid, a determination of the presence of anemia, thyroid disorder and/or vitamin D deficiency, and treatment options.
Treatments for Fibroids
Options for treating fibroids include observation with annual surveillance, addressing symptoms medically using non-steroidal anti inflammatory medication (NSAIDs) such as ibuprofen or naproxen, Tranexamic Acid, oral birth control, DepoProvera injections, Intrauterine device (IUD), Gonadotropin releasing hormone antagonists like Oriahnn and Myfembree and Gonadotropin releasing agonist like Lupron injections. In addition, there are minimally invasive uterine sparing treatment options such as uterine fibroid embolization, ultrasound assisted radiofrequency energy treatments such as acessa and sonata. There are uterine sparing surgeries called myomectomy (removal of fibroids) that can be performed vaginally via hysteroscopy, laparoscopy, robotically and/or open. Lastly, there is the hysterectomy (removal of the womb) which can be performed vaginally, laparoscopically, robotically and abdominally/ open.
A discussion with your gynecologist should include these treatment options as they pertain to you. If you are unsatisfied with the breadth of options offered or the reasoning for why you are a candidate for each option, seek a 2nd opinion. You should have a clear idea why you and your physician have chosen a specific therapy and how often you should follow up. You should also understand how your plan affects your fertility.
Fibroid Myths
Although social media has been a tremendous platform to spread information quickly there is a lot of misinformation floating around. Here are some myths you should be aware of:
fibroids can be cured by herbal teas and potions
Uterine tissue is responsive to herbs but not always in a positive way. These concoctions are not just ineffective, they are dangerous as they can cause the uterine tissue to become overactive and can affect other parts of the reproductive system such as the ovaries, and vagina.
there are physical exercises including yoga poses that can cure fibroids
A moderate to high intensity physical exercise program is encouraged in all humans with uteruses including those with fibroids after being cleared from a cardiac standpoint. Many physical exercises do relieve symptoms of fibroids and are useful in that sense. However, there are no exercises that have been proven to shrink or eliminate fibroids.
It is advisable to share any remedies/ approaches you are utilizing including dietary plans with your Ob/Gyn as you take a shared approach in addressing your fibroids.
REFERENCES
Baird DD, Dunson DB, Hill MC, Cousins D, Schectman JM. High cumulative incidence of uterine leiomyoma in black and white women: ultrasound evidence. Am J Obstet Gynecol. 2003 Jan;188(1):100-7. doi: 10.1067/mob.2003.99. PMID: 12548202.
Eltoukhi HM, Modi MN, Weston M, Armstrong AY, Stewart EA. The health disparities of uterine fibroid tumors for African American women: a public health issue. Am J Obstet Gynecol. 2014 Mar;210(3):194-9. doi: 10.1016/j.ajog.2013.08.008. Epub 2013 Aug 11. PMID: 23942040; PMCID: PMC3874080.
Jacoby VL, Fujimoto VY, Giudice LC, Kuppermann M, Washington AE. Racial and ethnic disparities in benign gynecologic conditions and associated surgeries. Am J Obstet Gynecol. 2010 Jun;202(6):514–21. Epub 2010 Apr 28.
Wechter ME, Stewart EA, Myers ER, Kho RM, Wu JM. Leiomyoma-related hospitalization and surgery: prevalence and predicted growth based on population trends. Am J Obstet Gynecol. 2011 Nov;205(5):492.e1–5. Epub 2011 Jul 20
Yu, Onchee et al. A US population-based study of uterine fibroid diagnosis incidence, trends, and prevalence: 2005 through 2014. American Journal of Obstetrics & Gynecology, Volume 219, Issue 6, 591.e1 - 591.e8